Iron Chelators as a Promising, Less Invasive Approach for Subarachnoid Hemorrhage
Subarachnoid hemorrhage (SAH) is a devastating form of hemorrhagic stroke with high mortality and long-term neurological consequences for survivors. While advances in surgical and critical care management have improved outcomes, treatment options that directly target the underlying biochemical damage after SAH remain limited. During the University of Florida Spring Undergraduate Research Symposium in 2023, I presented a literature-based research poster exploring iron chelation therapy as an emerging and potentially less invasive therapeutic strategy for SAH. It was one of the highlights of my undergraduate research experience, so I am excited to share it here to commemorate the work of my team!
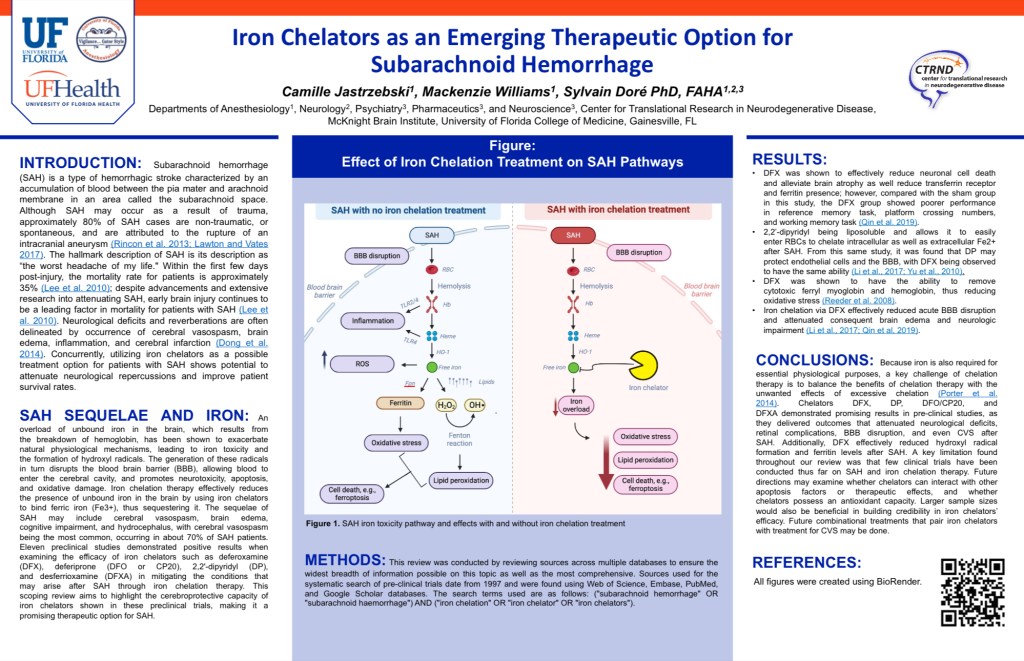
After SAH, the breakdown of red blood cells releases free iron into the brain. This excess iron drives oxidative stress, inflammation, lipid peroxidation, and ultimately neuronal cell death through mechanisms such as ferroptosis. These processes contribute to blood–brain barrier disruption, brain edema, vasospasm, and long-term cognitive impairment. My work synthesized preclinical evidence showing that iron chelators—such as deferoxamine (DFX), deferiprone (DFP), and 2,2′-dipyridyl (DP)—can bind excess iron and interrupt this toxic cascade.
Across multiple animal and cellular models, iron chelation was associated with reduced oxidative stress, preserved blood–brain barrier integrity, decreased neuronal cell death, and improved neurological outcomes following SAH. Importantly, these treatments act downstream of the initial hemorrhage, targeting secondary brain injury rather than the bleed itself. This positions iron chelation as a potential adjunct or alternative to more invasive interventions, especially for limiting delayed neurological damage.
Although this research was not formally published, it remains highly relevant. Iron-mediated toxicity continues to be an active area of investigation in stroke and neurodegenerative disease, and iron chelators are already FDA-approved for other clinical indications. This raises the possibility of repurposing existing drugs for SAH treatment—an approach that could shorten translational timelines and reduce patient risk compared to novel surgical or experimental therapies.
Sharing this work is important to me because it highlights how targeting biochemical pathways, rather than solely structural damage, may offer new avenues for treating complex neurological injuries. As research continues to explore less invasive, mechanism-driven therapies for brain injury, iron chelation remains a promising strategy worthy of further investigation.
Leave a comment